
Bariatric and Metabolic Surgery
Department of Bariatric and Metabolic Surgery
This surgery has been performed in the west since 1980’s. Now it has become popular in Asia. The long term results (>10 years) have proved that these surgeries are safe & effective. A significant sustained weight loss i.e. 60-90% is proved with 70-96% improvement in Obesity associated diseases.

Understanding the Comorbidities associated with Obesity
Insulin resistance is seen in obese persons as the tissue becomes refractory to regular amount of insulin secreted & requires more & more insulin. Ultimately this is a stage when pancreas can no longer produce insulin i.e., it gets burnt out & overt Diabetes Mellitus sets in.
Obesity produces a pro inflammatory state in the body causing the body to secrete more adrenaline & stress hormones. Increased abdominal fat produces intra abdominal hypertension which in turn affects the renin angiotensin system responsible for B. P. control.
Lipid metabolism is affected causing increased free fatty acid levels & cholesterol levels.
Excess fat is deposited in the liver known as Nonalcoholic steatohepatitis which is responsible for liver cirrhosis in later life.
Increased weight & increased uric acid levels cause joint pain. A patient with joint pain cannot exercise, hence the vicious cycle of weight gain which makes the joint pain continue.
Due to fat deposition around the neck the airway size is reduced. During sleep the tongue falls back obstructing the airway. This produces impaired alveolar ventilation & daytime somnolence. OSA is responsible for pulmonary arterial hypertension & ventricular hypertrophy, it is also responsible for sudden death in few morbidly obese patients.
Obesity causes polycystic ovarian disease (PCOD) which hampers ovulation. Sexual activity impairment due to obesity is another responsible factor.
Obesity is associated with Endometrial, breast, pancreatic & colonic cancer in later life. Obese patients have depression due to discrimination at workplace as well as altered self esteem.
What are the Surgical procedures performed for Morbid Obesity ?
Sleeve Gastrectomy
This is the most popular surgery worldwide. In this procedure stomach volume is reduced to 200-250ml which produces a restrictive component. Removal of fundus abolishes hunger surge. 70-80% of excess weight loss is expected.
It is a restrictive form of surgery which abolishes the ghrelin hormonal surge thereby preventing hunger induced food intake. It has been observed that it accelerates the gastric emptying thereby inducing hormonal changes i.e: increased GLP-1 thereby improving the glucose levels in diabetic patients. It Produces 60-80% of excess weight at 1 – 1.5 years
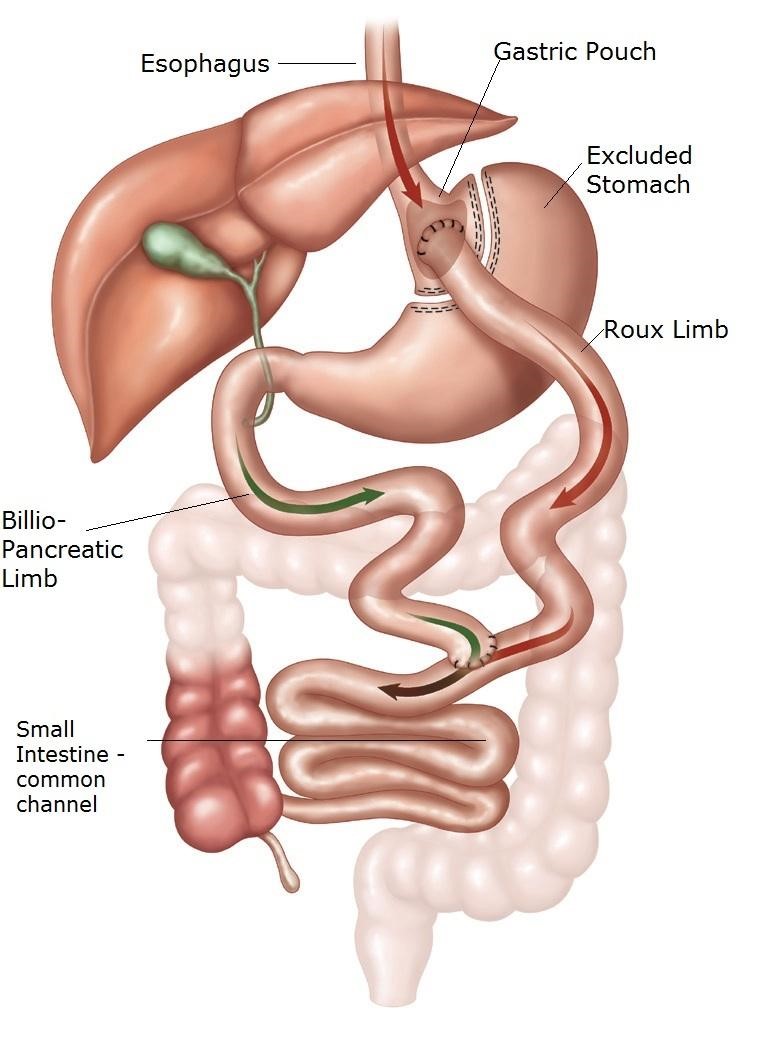
Gastric Bypass
In this surgery a small pouch (15-20 ml) is created & 100-150 cm of small intestine from the duodeno jejunal flexure is bypassed. So it has a restrictive & malabsorptive component which produces 80-90% of excess weight loss. Good for patients with severe comorbidities.
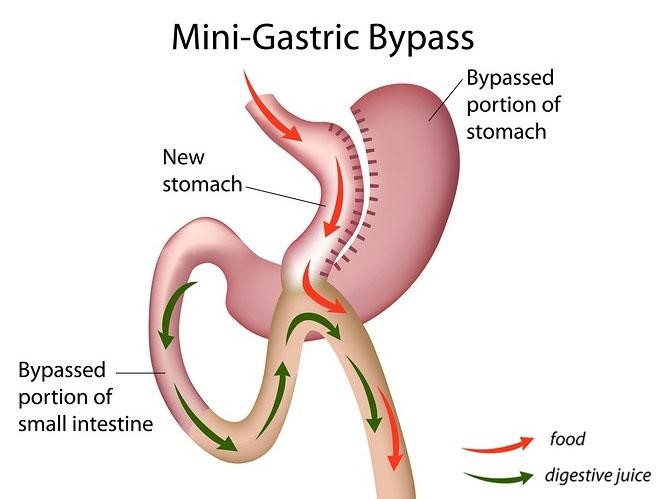
Mini Gastric Bypass
This is a form of bypass which has recently gained popularity in India. The diabetes remission rates have been to the tune of 80-90% with this procedure. Patients need to take iron, multivitamin & calcium supplements for prolonged time long after this procedure.
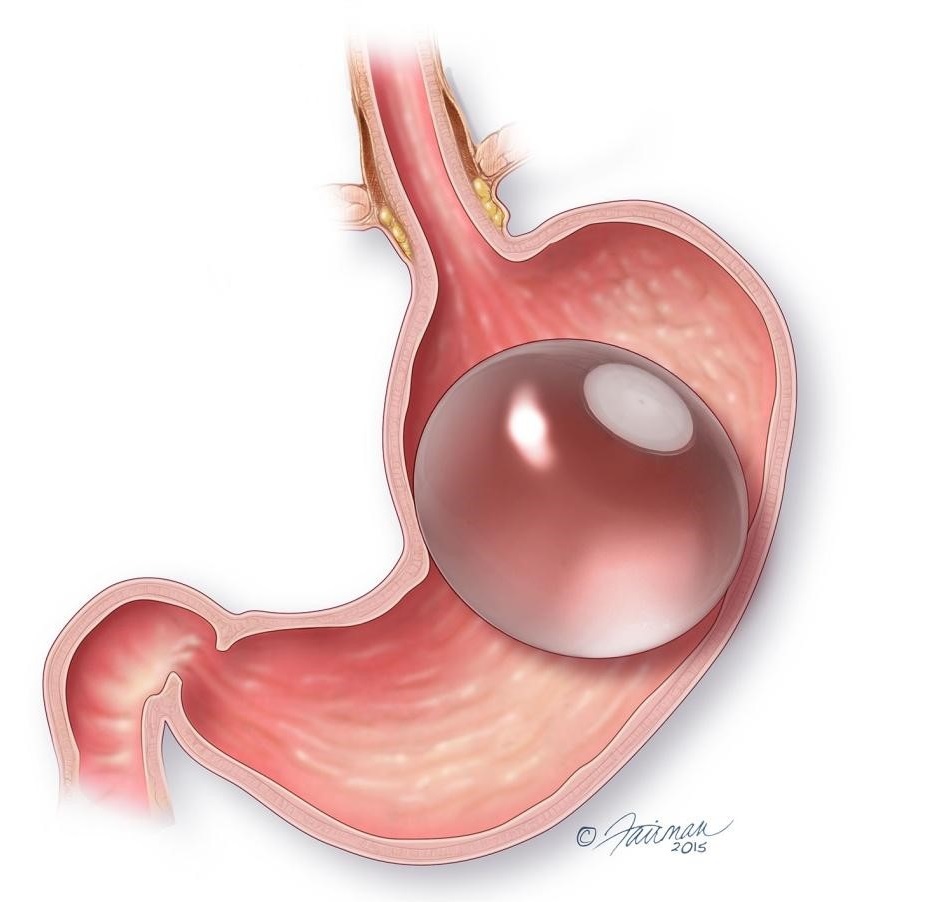
Non Surgical Weight loss - Intra gastric balloon
The Intra-gastric balloon is a non-surgical procedure where a silicon balloon is placed inside the abdomen endoscopically which makes a patient feel full. It could be an adjustable or non-adjustable balloon. Adjustable balloons are typically placed for 1 year whereas non-adjustable are placed for 6 months
It can be a good option for patients with BMI less than 32.5 or those high risk superobese patients with BMI more than 60 or 70 where balloon acts as a first stage procedure done to reduce the comorbidity severity and produce significant weight loss prior to definitive surgery.
Some Common Questions
- Patients with BMI > 37.5 without any diseases.
- Persons with BMI > 32.5 with any 2 comorbid diseases.i.e; Diabetes, hypertension, infertility, joint pains, obstructive sleep apnea, hyperlipidemia, fatty liver, hyperuricemia, impaired sexual function.
- Persons with BMI > 27.5 with uncontrolled comorbidities even with best medical management for example – Persons with uncontrolled blood sugar levels even with insulin & antidiabetic medications.
- Age between 18-65 years and well motivated person.
- Patients with chronic alcoholism, substance abuse.
- Patients unfit for general anaesthesia, portal hypertension.
- Unmotivated persons, severe psychiatric illness.
- Duodenal exclusion via surgery improves pancreatic function.
- As the food transit time is shortened i.e. food is delivered early into the small intestine, GLP-1 hormonal levels rise & this controls sugar via pancreas.
- Surgical procedure reduces weight which reduces insulin resistance.
This is performed laparoscopically under general anaesthesia. 3-5 small 1-2cm incisions are made on the patient’s abdomen. Laparoscopic surgery also known as keyhole surgery has an advantage of less pain, better cosmesis, early recovery & discharge.Patient needs to do some preliminary investigations followed by a liquid diet regime for 3 days to 7 days. Hospitalization is for 3-5 days & patients can resume work within 10-15 days.
Bariatric surgery is different from liposuction. It is a Gastrointestinal Surgery which produces significant weight loss. Liposuction refers to procedures where superficial abdominal fat is removed. Mainly done who require cosmesis. Weight loss expected is less.
This surgery has risks as any other laparoscopic surgery. There is a small <1% Risk of anastomotic leak & bleeding.> Modern anesthesia has made this procedure safe. Few patients may have skin laxity or nutritional deficiencies if adequate protein intake & diet is not followed.
Weight loss is more with malabsorptive procedures whereas less in predominantly restrictive procedures. A 60-90 % of excess weight loss is expected over 1-1.5 years time period.
Improvement is seen in 96% of Diabetics, 80% of Hypertensive patients. Resolution is seen in 85-90% of patients with hyperlipidemia & hyperuricemia,joint pain .
27% of obese patients will develop new onset Diabetes Mellitus as compared to 4% in normal patients over 10 years. Quality of life improves with weight loss for example- increased mobility & work productivity.
Central Government employees can avail the benefit of a free surgery under CGHS Scheme
Few of the patients do get insurance claims and IRDA has made it mandatory to cover this surgery under the insurance. Apart from that there are few financial institutes who offer monetary help to the needy as a loan on EMI basis. PMC also helps eligible Pune residents monetarily.
FAQ's
What is Bariatric Surgery?
How much weight can I expect to lose after undergoing bariatric surgery?
The amount of weight you can expect to lose after bariatric surgery varies depending on several factors including the type of procedure, your starting weight, lifestyle changes, and adherence to post-surgery guidelines. On average, patients may lose 60 to 90% of their excess body weight within the first year following surgery. However, consulting with your healthcare provider for personalized expectations based on your circumstances is essential.
How to Choose the Best Bariatric Surgery Hospital in Pune?
When selecting the best bariatric surgery hospital in Pune, it’s crucial to consider several factors. Look for hospitals with experienced bariatric surgeons, state-of-the-art facilities, comprehensive pre-operative and post-operative care programs, success rates, patient testimonials, and accreditation. Additionally, ensure that the hospital offers personalized treatment plans tailored to your specific needs and provides ongoing support throughout your weight loss journey.
Does Bharati Hospital Pune have qualified bariatric surgeons?
Yes, Bharati Vidyapeeth Hospital Pune boasts a team of highly qualified and experienced bariatric surgeons who are dedicated to providing exceptional care to patients seeking weight loss solutions. As one of the top bariatric surgery hospitals in Pune, Bharati Hospital prides itself on its skilled medical professionals who utilize advanced techniques and technologies to deliver safe and effective surgical outcomes.
Why is Bharati Hospital the best choice for Bariatric Surgery in Pune?
Bharati Hospital stands out as the premier choice for bariatric surgery in Pune, Maharashtra due to its unparalleled commitment to patient care, renowned team of bariatric surgeons, cutting-edge infrastructure, and track record of successful outcomes. As a leading bariatric surgery hospital in Pune, Bharati Hospital prioritizes patient safety, comfort, and long-term success, offering comprehensive support services and personalized treatment plans tailored to each patient’s unique needs.


